Learn about infections, sepsis, and the immune system as an ideal diagnostic
Acute Infection and Sepsis
Visits to the emergency department due to acute infection symptoms are common
Acute infections are extremely common. When their symptoms are sufficiently severe or access to care elsewhere is not available, patients visit the emergency department for diagnosis and treatment. We estimate over 20 million and 15% of all ED visits relate to symptoms of acute infections.1
Patients coming to the emergency department are presumed ill until proven otherwise. Patients suspected of infection are no different. As a result, physicians usually assess how ill is the patient and whether the illness is due to an acute infection.
A diagnosis requires both insights.
Typical approach used to assess patients coming to the emergency department2
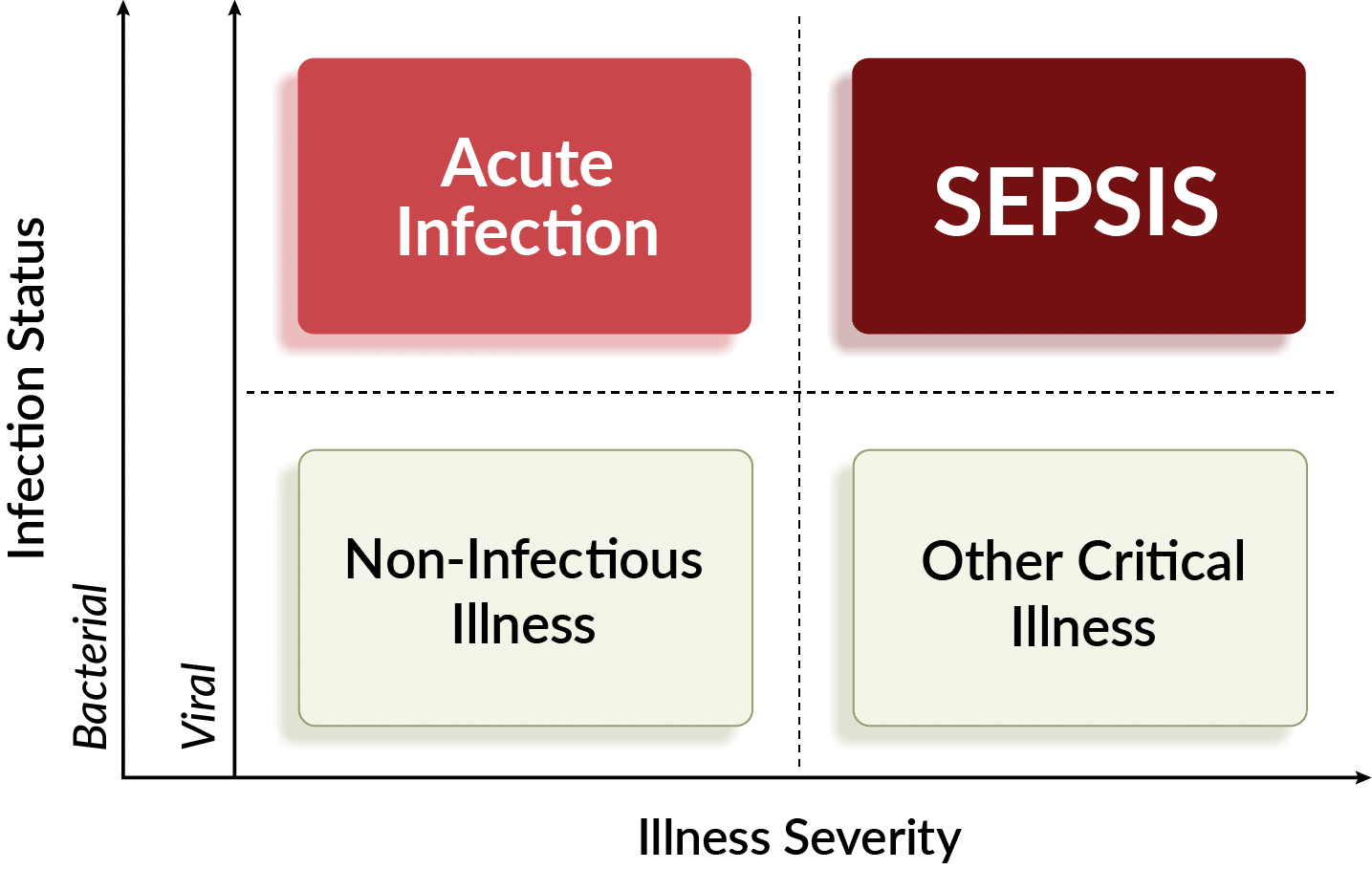
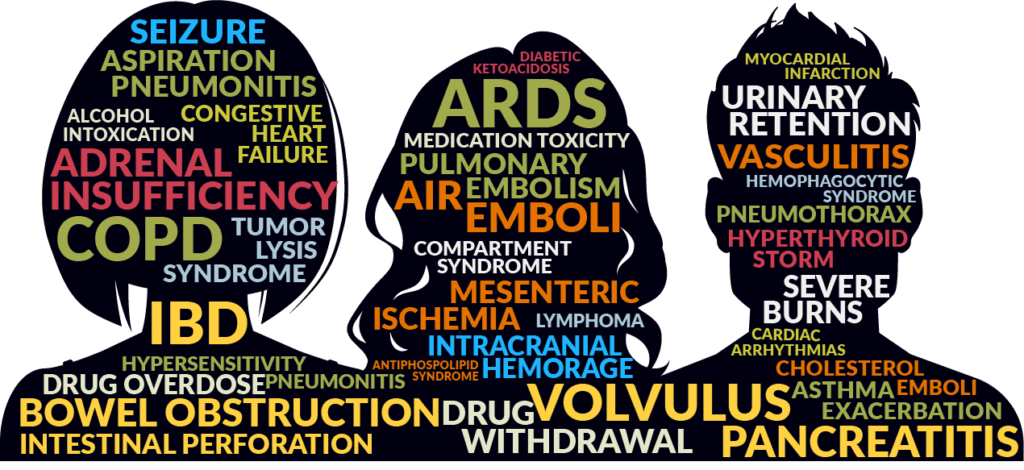
NON-INFECTIOUS illness & other critical illness
When patients are extremely sick, ruling out infection is vital in order to determine the illness cause and provide the right treatment. For example, patients in heart failure or experiencing COPD exacerbations require different treatments than septic patients.
About 20% of non-severely ill patients with symptoms of infection do not actually have one. Their symptoms may by caused by allergy, asthma, non-severe COPD exacerbation, or other disease. Ruling out an infection and narrowing down the actual cause of illness can be important to provide peace of mind, reduce resource utilization and limit escalation of disease.6
ACUTE INFECTION
Infected patients without sepsis are also challenging to diagnose in the Emergency Department
While sepsis is gravely concerning, most patients with infections in the ED do not have life threatening infection. Knowing whether an infection is bacterial or viral impacts antibiotic prescribing, discharge versus admission and other treatment decisions. Better tests that can more accurately rule-out bacterial infections may help reduce unnecessary antibiotic usage, which occurs an estimated 39% of the time.7
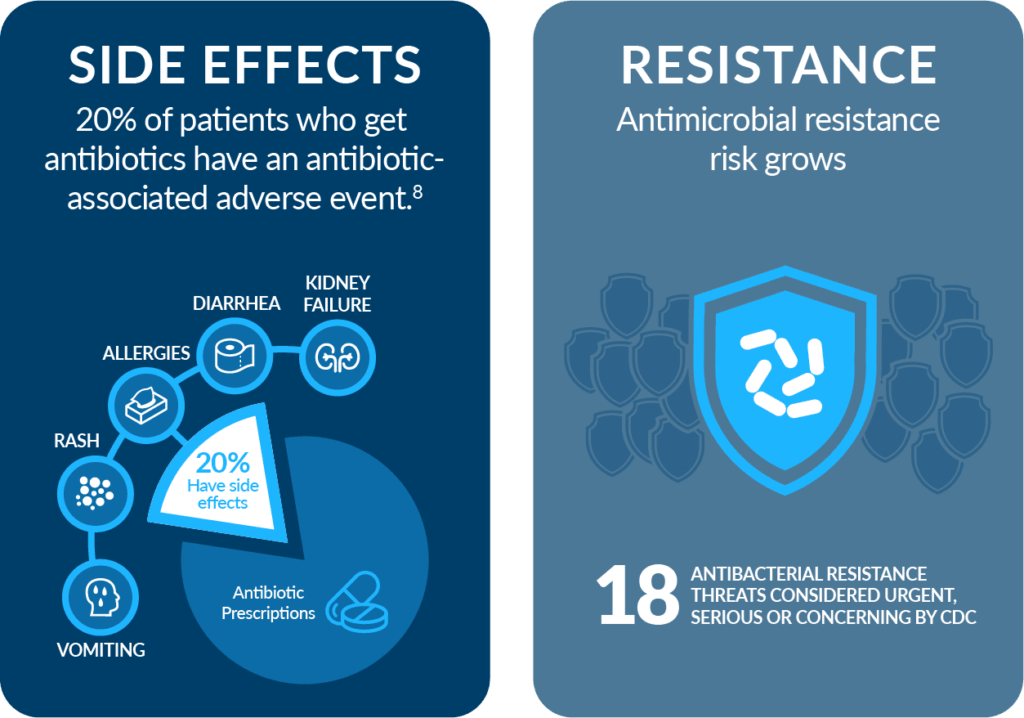
Inappropriate antibiotic prescribing can have significant consequences as patients on antibiotics experience adverse events 20% of the time and excess antibiotic use risks an increase in antimicrobial resistance.8
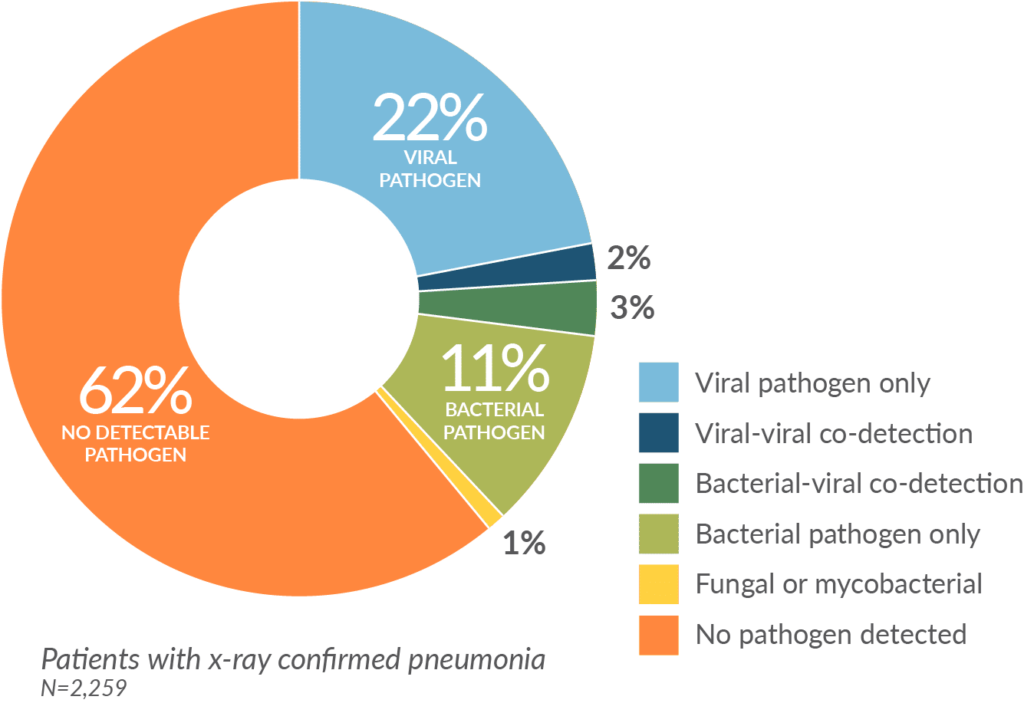
Nevertheless, many are challenging to manage. In many patients, common infections such as those located in the respiratory, abdominal, skin and soft tissue, or urinary tract often do not yield positive results on routine pathogen tests. For example, in a study published in the New England Journal of Medicine of confirmed pneumonia patients, 62% did not have positive microbiology.9
SEPSIS
A concerning and dangerous subset of patients with acute infections
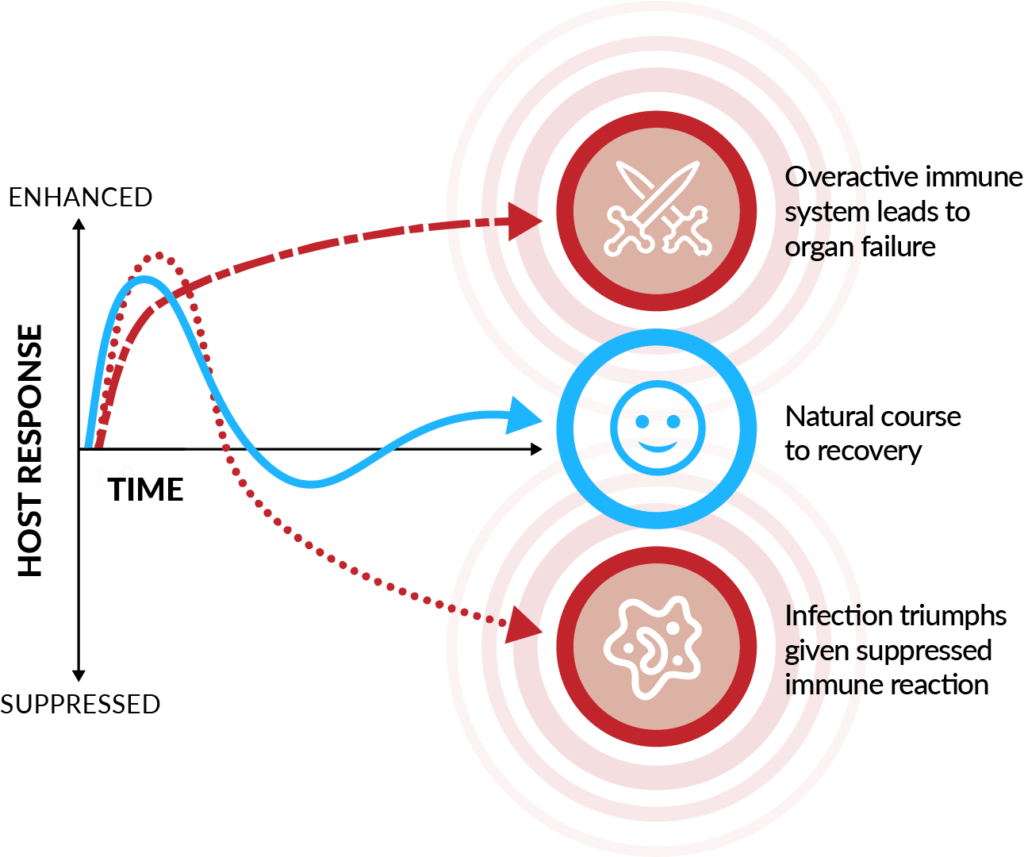
Sepsis is a dysregulated immune response that can be triggered by any acute infection. It can lead to tissue damage, organ failure, and worse. With the highest hospital mortality of any diagnosis, sepsis accounts for nearly half of in-hospital deaths. Identifying sepsis quickly is vital as risk of death increases by 7% for every hour in delay of antibiotics treatment.10
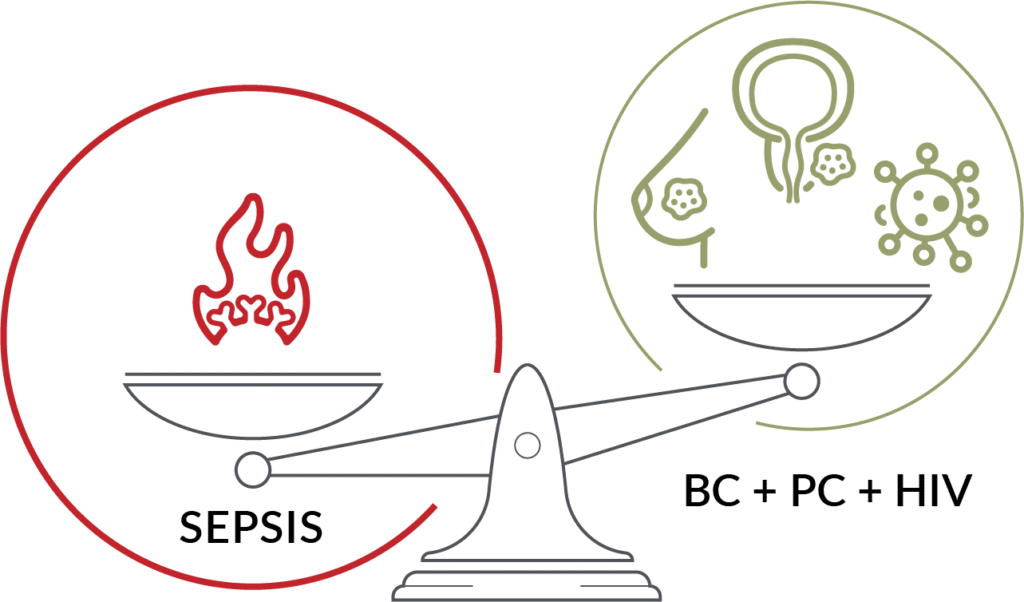
An estimated 1.7 million of the 20 million patients assessed for infection are diagnosed with sepsis.1,11,12 Given that over 270,000 die from sepsis, more than breast cancer, prostate cancer, and HIV/AIDS combined, it garners great urgency and focus by Emergency Medicine physicians and hospital staff.13
A fraction of septic patients are bacteremic

Only 10% of hospitalized patients have a bloodstream infection
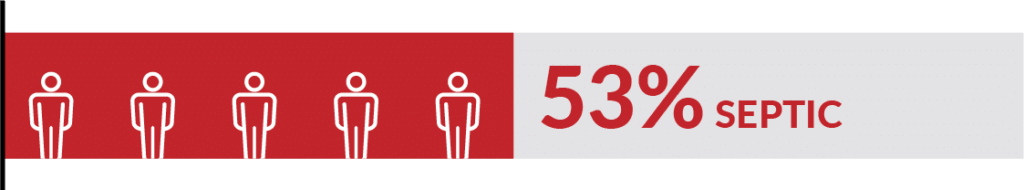
Only 53% of septic patients have a bloodstream infection
Sepsis ≠ Bloodstream Infection
IMMUNE RESPONSE
The Power of the Immune Response
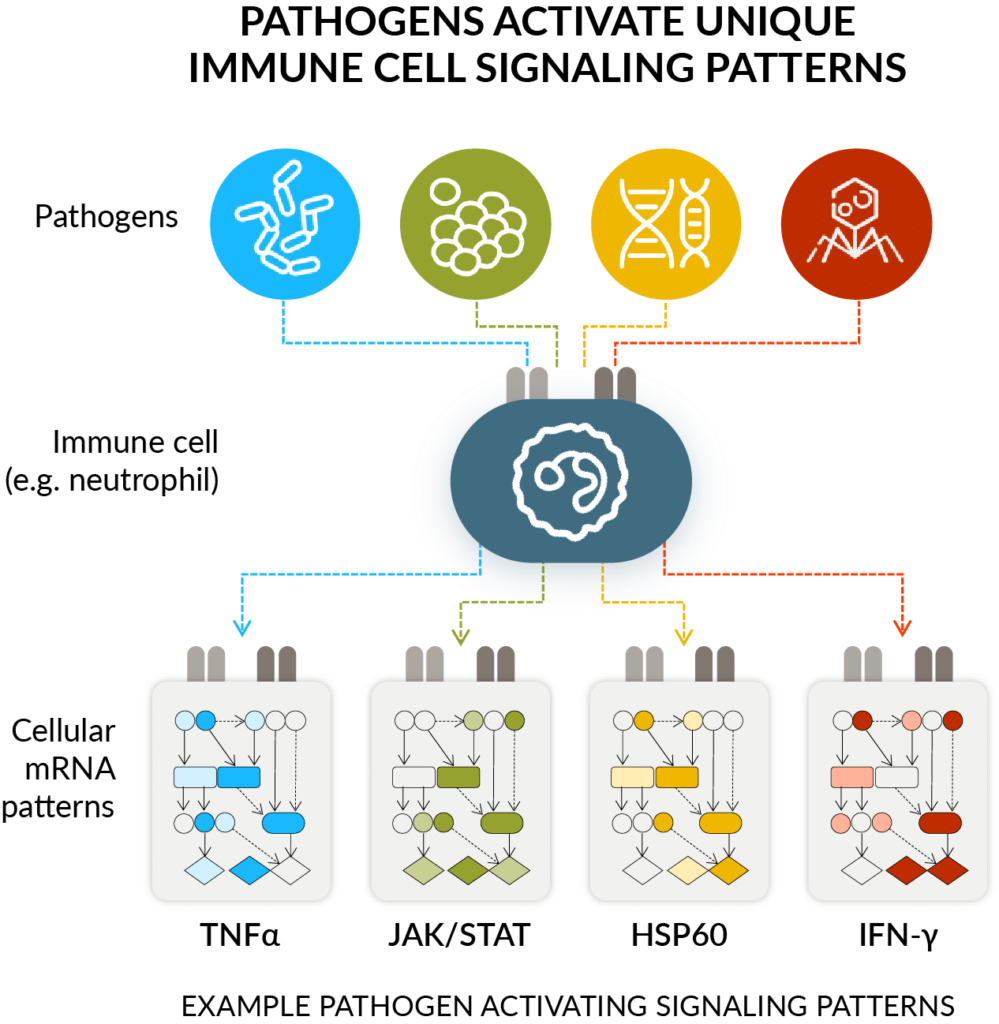
Our immune system has developed targeted responses to different types of infections and other diseases over millions of years. Depending on the insult, the immune system will react differently. Its response to a serious bacterial infection is different than to a non-serious viral one or non-infectious reaction, like an allergic reaction.
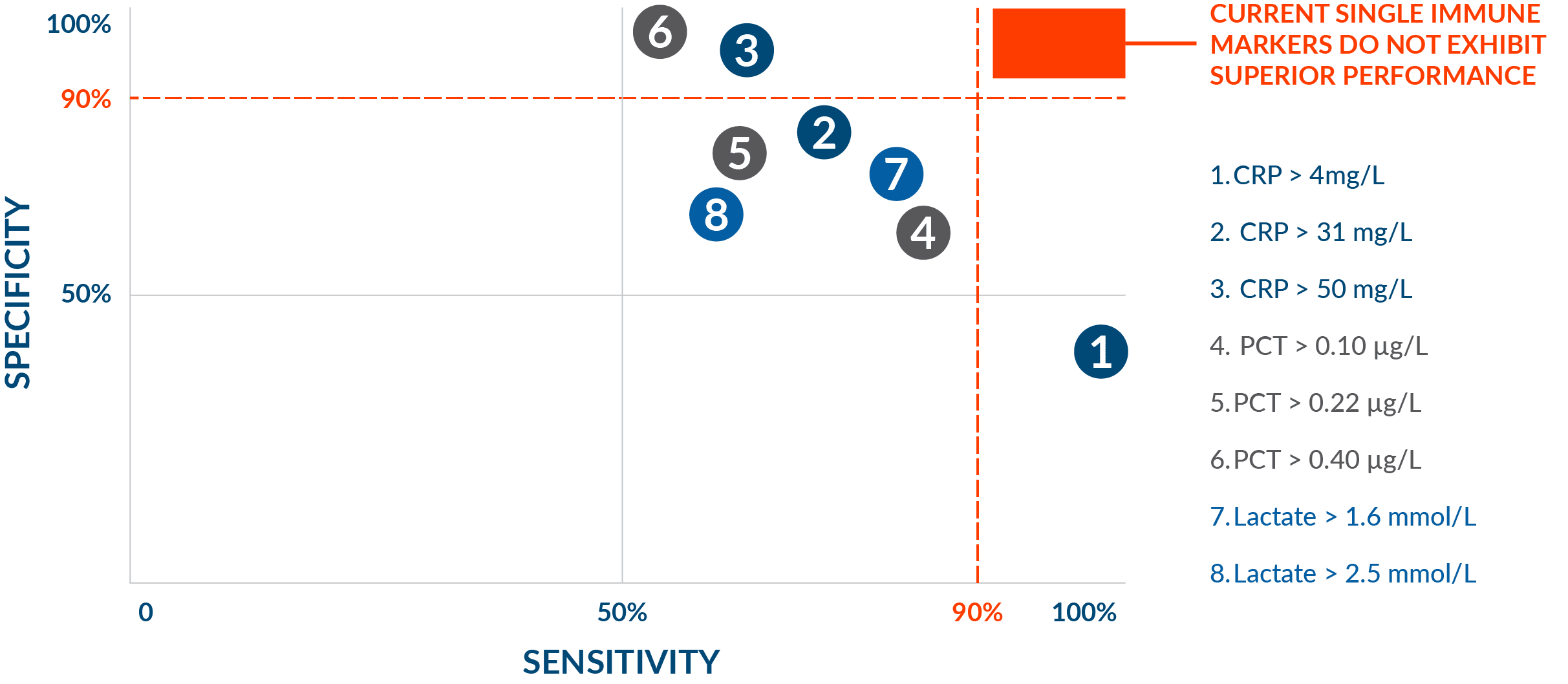
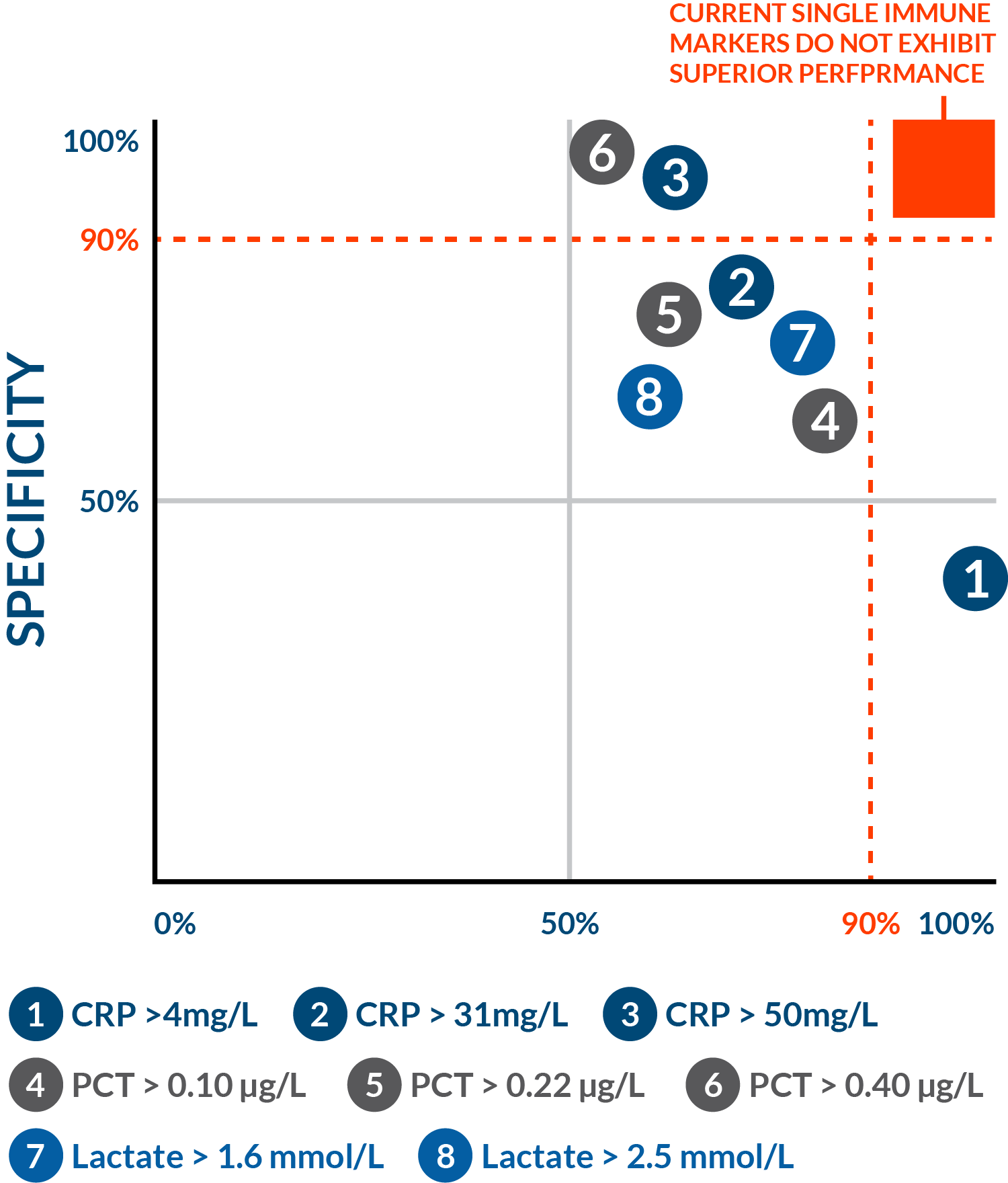
Traditional immune markers have not been good enough
The clinical performance of traditional biomarkers like CRP, lactate, and PCT limits their ability to be reliable rule-in or rule-out tests. These general markers of inflammation or insult have been widely adopted given the need to determine the presence, type, and severity of infection. Nevertheless, unmet needs for more accurate tests, with better sensitivity and specificity performance, remain.
Host response opens new doors in the clinical setting
This century, the molecular revolution has included the ability to rapidly measure many markers at once (thanks to advances in lab techniques) and gain insights into what they mean (as a result of progress in bioinformatic techniques).
The combination of these two technological advancements promises to provide clinicians what they want: rapid tests that are highly accurate (high sensitivity and high specificity) that enable confident infectious disease presence and severity prognosis.
Explore how the immune system can address the challenges of diagnosing acute infections
Visit hostreponsedx.comGeneral education website relating to the power of host response diagnostics to address unmet needs in diagnosing acute infection and sepsis in the emergency department.
MACHINE LEARNING
Transforming diagnostics with machine learning and artificial intelligence
Machine learning and artificial intelligence have the potential to transform nearly every facet of healthcare, and prognostics/diagnostics for acute care are no exception. When coupled with rapid profiling of patient host response from blood, ML/AI-driven models promise earlier and more accurate detection of the presence and type of infection, timely stratification of patients by the severity of their condition, and characterization of patients into molecular subtypes more amenable to different treatment strategies.
Ingredients for a Successful ML Program
At Inflammatix ML, we understand that bringing world-class ID diagnostics to the point of care demands a holistic approach. Our highly interdisciplinary team draws on decades of experience in academic and industrial science with backgrounds ranging from applied statistics, computer science, engineering, bioinformatics, and software development. We pursue both methodological and applied research directions, developing novel models and methods when the need arises but also investigating the feasibility of the ‘tried-and-true’ as well as the ‘latest-and-greatest’.
We prioritize sharing our work and insights with the broader research community in both publications and international conferences. We continue to grow and curate one-of-a-kind patient datasets, leveraging information at multiple scales to guide selection of high-performing biomarkers and diagnostic classifiers. We engage stakeholders across the company and the medical community to help our test achieve leading performance and optimal integration with clinical workflows and decision-making.
Systems for diagnostic classifier development
Patient host response, as measured by expression of targeted mRNA biomarkers from blood, can vary from patient to patient. Previous approaches have developed host response signatures and classifiers that tend to generalize poorly, owing to biomarker selection and classifier training and validation on a limited, unrepresentative set of patient observations from a single study or hospital. Pooling of data across multiple studies has proven effective in producing more generalizable host response signatures and classifiers but introduces other methodological challenges.
Hyperparameter optimization of diagnostic classifiers
An essential step in classifier selection is hyperparameter optimization, or the identification of values for a classifier’s hyperparameters that optimize some objective function (e.g., performance in cross-validation). While conventional methods of grid search and random sampling can still be effective, more sophisticated approaches such as Bayesian optimization16 and Hyperband17 have demonstrated gains in terms of both performance and efficiency (i.e., producing high-performing classifiers with fewer evaluations of candidate hyperparameterizations) on a range of ML benchmarks.
Fairness in diagnostics
Recent studies have increasingly shown potential for performance disparities of deployed ML systems associated with demographic characteristics of the populations those systems are intended to serve. These disparities can have harmful downstream consequences when the system outputs are used to guide or replace human decision-making and can arise for reasons such as low representation of certain subgroups in training data or choices of features or training objectives that accentuate such disparities.
Want more details on our ML/AI progress?
Explore the ml blogINFLAMMATIX ADVOCACY
Committed to Non-Profit and Government Partners
Inflammatix is committed to end sepsis through better diagnosis. We stand with these distinguished organizations, committed to solving sepsis and fighting antimicrobial resistance.
- HCUPnet, Healthcare Cost and Utilization Project. Agency for Healthcare Research and Quality, Rockville, MD.
- Prescott H.C., et al., Improving Sepsis Treatment by Embracing Diagnostic Uncertainty. Ann Am Thorac Soc. 2019 Apr;16(4):426-429. doi: 10.1513/AnnalsATS.201809-646PS. PMID: 30883190; PMCID: PMC6441693.
- Kellum, JA, et.al., Subtypes and Mimics of Sepsis, Critical Care Clinics, Volume 38:2, p 195-211, April 2022.
- Lengquist M et al., Sepsis mimics among presumed sepsis patients at intensive care admission: A retrospective observational study. Infection 2024 Jan 27; [e-pub]
- Chest Sepsis Mimics Infographic, Last updated June 27, 2023.
- Rudd, K.E., Kissoon, N., et al., The global burden of sepsis: barriers and potential solutions. Crit Care 22, 232 (2018).
- Timbrook, T. T., et. al., 2018, Assessments of Opportunities to Improve Antibiotic Prescribing in an Emergency Department: A Period Prevalence Survey: Adis Journals, doi:10.6084/m9.figshare.5828151.v1.
- Tamma PD, et al., JAMA Intern Med. 2017 Sep 1;177(9):1308–1315.
- Jain S, et. al., Community-Acquired Pneumonia Requiring Hospitalization among U.S. Adults, N Engl J Med 2015;373:415-427.
- Seymour CW et al., Time to treatment and mortality during mandated emergency care for sepsis. N Engl J Med 2017 May 21; [e-pub].
- Rhee C, Dantes R, Epstein L, et al; CDC Prevention Epicenter Program. Incidence and trends of sepsis in US hospitals using clinical vs claims data, 2009-2014. JAMA. 2017;318(13):1241-1249. doi:10.1001/jama.2017.13836
- https://www.cdc.gov/sepsis/what-is-sepsis.html#anchor_1547214418, Last reviewed: August 24, 2023.
- Sepsis, Content reviewed: September 2023
- Colburn, et al., Does This Adult Patient With Suspected Bacteremia Require Blood Cultures?. JAMA. 2012;308(5):502–511.
- Blauwkamp, T.A., et al., Analytical and clinical validation of a microbial cell-free DNA sequencing test for infectious disease. Nat Microbiol 4, 663–674 (2019).
- Snoek, J., et al., Practical Bayesian Optimization of Machine Learning Algorithms, NeurIPS Proceedings NIPS 2018.
- Li et al., 2018 Hyperband: A Novel Bandit-Based Approach to Hyperparameter Optimization, Journal of Machine Learning Research 18 (2018) 1-52.